New research at Arizona State University is investigating the evolution and function of the protein TRPM8 with the goal of developing non-addictive painkillers that avoid side effects associated with temperature regulation, potentially revolutionizing the treatment of chronic pain.
Menthol can be detected before the sensation of cold, suggesting that different activation mechanisms can be distinguished. This differentiation opens up possibilities for novel pain treatments that avoid undesirable thermal side effects.
Millions of people around the world suffer from chronic pain and many of the existing treatments are based on opioids, which carry significant addiction and overdose risks. Developing non-addictive pain relief options could change the way pain is treated. Recent research into a human protein that controls the sensation of cold is paving the way for new painkillers. These innovative drugs aim to relieve pain without changing body temperature or carrying addiction risks.
A new study was published on June 21 in the journal Scientific advancesled by Wade Van Horn, professor in the School of Molecular Sciences and the Biodesign Center for Personalized Diagnostics at Arizona State University, has shed new light on the key human cold and menthol sensor, TRPM8 (Transient Receptor Potential Melastatin 8). Using techniques from many fields such as biochemistry and biophysics, their study revealed that it was a chemical sensor before it became a cold temperature sensor.

The team used ancestral sequence reconstruction to study ancient TRPM8 proteins, finding new ways to relieve pain without the side effects of previous TRPM8-targeted treatments. This research is an example of how evolutionary biology and modern pharmacology can work together to improve chronic pain treatment. Image credit: ASU/ Wade Van Horn
“If we understand how to separate the chemical perception of cold from the actual perception of cold, we could theoretically create side-effect-free drugs,” said Van Horn, whose research focuses on membrane proteins involved in human health and disease. “By understanding the evolutionary history of TRPM8, we hope to help develop better drugs that provide relief without the dangerous side effects associated with current painkillers.”
The role of TRPM8 in pain
When a person touches a metal table and it feels cold, the human body activates TRPM8. For cancer patients taking certain types of chemotherapy drugs, touching a table can be painful. TRPM8 is also involved in many other types of pain, including chronic neuropathic and inflammatory pain.
By better understanding these peculiarities of chemical cold sensation compared to physical cold sensation, scientists can provide targeted relief without triggering the temperature regulation side effects commonly observed in TRPM8 clinical trials for pain management.
For their research, the team used ancestral sequence reconstruction, a kind of time machine for proteins, and assembled the family tree of TRPM8 that exists today. Using this information, the team then determined what the proteins of long-extinct animals might have looked like.
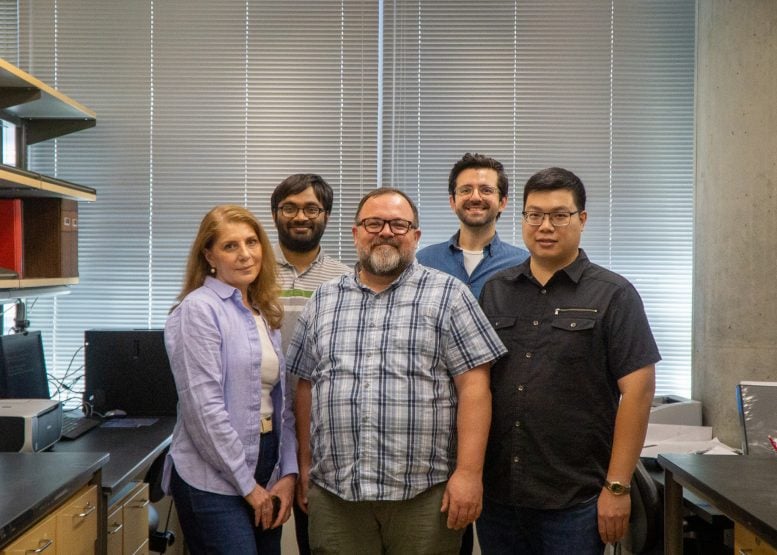
A study published June 21 in Science Advances led by Wade Van Horn, a professor in the School of Molecular Sciences and the Biodesign Center for Personalized Diagnostics at Arizona State University (center), has revealed new insights into the key human cold and menthol sensor, TRPM8 (Transient Receptor Potential Melastatin 8). Image credit: ASU/David Rozul
Using computational methods, the researchers were able to recreate TRPM8 from primates, mammals and vertebrates. This allowed them to understand how TRPM8 has changed over hundreds of millions of years. They compared the sequences of current proteins and were thus able to predict the sequences of their ancient ancestors. In addition, by combining laboratory experiments and computational studies, the researchers were able to identify critical sites in TRPM8 that allow a clearer understanding of temperature perception, which can be tested in subsequent experiments.
“A comparative dynamics analysis of the original and human TRPM8 also supports the experimental data and will allow us to identify critical points in temperature sensing that we will soon test,” said Banu Ozkan, a professor in ASU’s Department of Physics who was involved in the study.
Advances in the study of original proteins
The team then expressed these original TRPM8s in human cells and characterized them using various cellular and electrophysiological techniques.
Ion channel in the cell membrane, 3D illustration.
“Ancestral protein-based studies allow us to focus on the most interesting lineage, such as human TRPM8, and address concerns that arise in drug discovery due to species differences such as those between mice and humans,” said study lead author Dustin Luu, a doctoral student in the ASU School of Molecular Sciences and currently a postdoctoral fellow at ASU’s Biodesign Center for Personalized Diagnostics.
Luu continued, “We surprisingly discovered that menthol perception occurred long before cold perception. The difference in the emergence and attenuation of these activation modes suggests that they are separate and can be disentangled through further research, enabling new pain therapies without the adverse side effects on heat perception and regulation that have plagued clinical trials using TRPM8 targets.”
As science continues to unravel more secrets of our biological mechanisms, studies like this one illustrate how evolutionary biology and modern pharmacology can work together to meet urgent medical needs and improve the quality of life of people with chronic pain.
Reference: “Evidence that the cold and menthol sensing functions of the human TRPM8 channel evolved separately” by Dustin D. Luu, Nikhil Ramesh, I. Can Kazan, Karan H. Shah, Gourab Lahiri, Miyeko D. Mana, S. Banu Ozkan, and Wade D. Van Horn, June 21, 2024, Scientific advances.
DOI: 10.1126/sciadv.adm9228